States' Collection of Medicaid Rebates from Drug Manufacturers
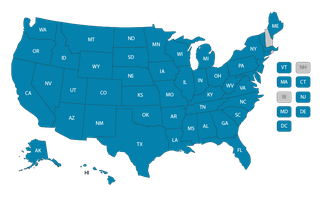
In this series of reports, OIG is determining whether each State billed and collected from pharmaceutical manufacturers the rebates they owe to States and Federal Government for outpatient drugs dispensed in the Medicaid program.
Most of the reports in this series of reports focus on traditional Medicaid (fee-for-service), looking at rebates for drugs administered by physicians in an office or hospital outpatient facility. Other reports focus on Medicaid managed care, some looking at just drugs administered by physicians and some looking at rebates for all outpatient drugs.
Nationwide Summary: State Agencies Could Be Obtaining Hundreds of Millions in Additional Medicaid Rebates Associated With Physician-Administered Drugs (A-07-23-06111)
Last updated February 13, 2026
