Report Materials
Why OIG Did This Audit
- Medicare does not generally cover routine foot care (RFC) services unless the enrollee has systemic medical conditions that increase the risk of infection or injury if the services are not performed by a medical nonprofessional (e.g., a podiatrist). Medicare assumes that the enrollee or a caretaker will perform these services.
- A 2002 OIG report found that Medicare inappropriately paid podiatrists for RFC services that were medically unnecessary and insufficiently documented. Because OIG has not reviewed podiatry services since that report, we conducted this audit to determine whether these compliance issues continued to exist in 2019 and 2020 (audit period).
- This audit examined whether podiatrists’ claims for RFC services related to a systemic condition complied with Medicare requirements.
What OIG Found
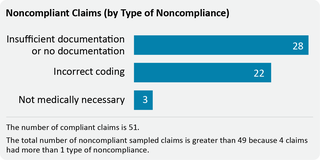
- Of the 100 sampled claims, 49 podiatrists’ claims for RFC services related to a systemic condition did not comply with Medicare requirements.
- During our audit period, CMS’s oversight may not have been sufficient to prevent improper payments.
- On the basis of our sample results, we estimated that of the $18.2 million paid by Medicare for our audit period, approximately $4.4 million did not comply with Medicare requirements.
What OIG Recommends
We recommend that CMS work with the Medicare Administrative Contractors to determine whether additional oversight is necessary to prevent payments for RFC services that did not comply with Medicare requirements, which amounted to an estimated $4.4 million for our audit period.
CMS concurred with our recommendation.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.