Report Materials
Why OIG Did This Audit
- For a covered outpatient drug to be eligible for Federal reimbursement under the Medicaid program’s drug rebate requirements, manufacturers must pay rebates to the States for the drugs.
- Prior OIG audits found that States did not always invoice and collect all rebates due for drugs administered to Medicaid managed-care organization (MCO) enrollees.
- This audit, one of a series, determined whether Pennsylvania complied with Federal Medicaid requirements for invoicing manufacturers for rebates for physician-administered drugs dispensed to MCO enrollees.
What OIG Found
- Pennsylvania generally complied with applicable Federal Medicaid requirements but did not invoice all rebate eligible physician-administered drugs dispensed to MCO enrollees.
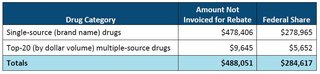
- Specifically, Pennsylvania did not invoice for rebates totaling $488,051 ($284,617 Federal share):
What OIG Recommends
We made three recommendations to Pennsylvania, including that Pennsylvania invoice for and collect from manufacturers rebates totaling $488,051 ($284,617 Federal share) for single-source and top-20 multiple-source physician-administered drugs and refund the Federal share of rebates collected. The full recommendations are in the report.
Pennsylvania agreed with all three recommendations.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.