Report Materials
Why OIG Did This Audit
- In March 2020, Congress enacted the Families First Coronavirus Response Act in response to the COVID-19 public health emergency, which required States to ensure that most individuals were continuously enrolled for Medicaid benefits (enrollees).
- The Consolidated Appropriations Act, 2023, ended the continuous enrollment condition. As a result, States had to conduct renewals, post-enrollment verifications, and redeterminations (Medicaid eligibility actions) for all enrollees, including terminating Medicaid enrollment of ineligible individuals.
- This audit of Utah is part of a series of audits examining whether States completed Medicaid eligibility actions during their unwinding periods in accordance with Federal and State requirements.
What OIG Found
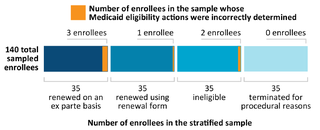
Of the 193,009 enrollees who had their Medicaid eligibility renewed or coverage terminated during April 1 through September 30, 2023 (audit period), we sampled 140 enrollees and determined that Utah incorrectly completed Medicaid eligibility actions for 6 enrollees.
On the basis of our sample results, we estimated that Utah incorrectly renewed eligibility or incorrectly terminated Medicaid coverage for 5,233 of the 193,009 enrollees during our audit period. We also estimated that Utah reported 15,269 of the 193,009 enrollees on the incorrect line of Utah’s monthly unwinding data reports to CMS during our audit period.
What OIG Recommends
We made four recommendations to Utah, including that it redetermine Medicaid eligibility for the six sampled enrollees identified as having incorrect eligibility determinations, provide periodic training to caseworkers, identify and correct data limitations we identified, and strengthen policies and procedures to provide for greater accuracy in the monthly unwinding data reports. The full recommendations are in the report.
Utah concurred with all our recommendations and described corrective actions it had taken or planned to take.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.