Report Materials
Why OIG Did This Audit
- In March 2020, Congress enacted the Families First Coronavirus Response Act in response to theCOVID-19 public health emergency, which required States to ensure most individuals were continuously enrolled for Medicaid benefits (enrollees).
- The Consolidated Appropriations Act, 2023, ended the continuous enrollment condition. As a result, States had to conduct renewals, post-enrollment verifications, and redeterminations (Medicaid eligibility actions) for all enrollees, including disenrolling individuals who were no longer eligible.
- This audit is part of a series that examined whether Ohio completed Medicaid eligibility actions during its unwinding period in accordance with Federal and State requirements.
What OIG Found
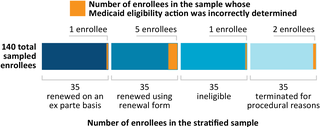
Of the 1,211,991 enrollees covered under our audit period (April 1 through August 31, 2023), we sampled 140 enrollees and determined that 9 enrollees had their Medicaid enrollment incorrectly determined.
On the basis of our sample results, we estimated that Ohio either incorrectly renewed or terminated Medicaid eligibility for 78,486 of the 1,211,991 Medicaid enrollees during our audit period.
What OIG Recommends
We recommend that Ohio:
- take appropriate action with respect to the incorrect Medicaid eligibility determinations identified in our sample,
- provide periodic training to caseworkers about verifying and documenting enrollees’ income during the renewal process, and
- provide additional training to caseworkers about using current information when conducting enrollee eligibility determinations.
Ohio concurred with all our recommendations and described actions that it has taken or plans to take in response to our recommendations.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.