2017 National Health Care Fraud Takedown

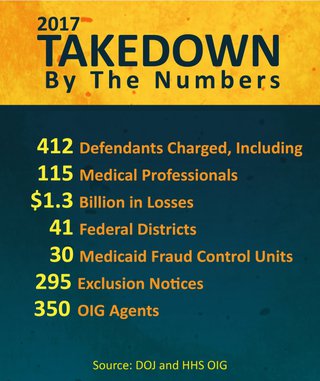
The Department of Health and Human Services Office of Inspector General, along with our state and federal law enforcement partners, participated in the largest health care fraud takedown in history in July 2017. More than 400 defendants in 41 federal districts were charged with participating in fraud schemes involving about $1.3 billion in false billings to Medicare and Medicaid. OIG also issued exclusion notices to 295 doctors, nurses, and other providers based on conduct related to opioid diversion and abuse.
Takedowns protect Medicare and Medicaid and deter fraud -- sending a strong signal that theft from these taxpayer-funded programs will not be tolerated. The money taxpayers spend fighting fraud is an excellent investment: For every $1.00 spent on health care-related fraud and abuse investigations in the last three years, more than $5.00 has been recovered.
Photo Gallery
2017takedown9.jpg 2017takedownimage21.jpg 2017takedownGearingup.jpg 2017takedownBriefing.jpg 2017takedownPerpwalk.jpgGraphics Gallery
2017takedownmc_excluded.jpg 2017takedownmc_by-the-numbers.jpg 2017takedowngeneral-overview.png 2017takedowndosage-amounts.png 2017takedownpatients.png 2017takedownprescribers.png 2017takedowndoj-oig-graphic.png- View a text-only version of these graphics
Additional Resources
- Press Release
- Medicare Fraud Strike Force
- Opioids in Medicare Part D: Concerns about Extreme Use and Questionable Prescribing
- National Health Care Fraud Takedown 2016
- Curbing the Abuse and Misuse of Controlled and Non-controlled Drugs in Medicare Part D and Medicaid
- Questionable Billing and Geographic Hotspots Point to Potential Fraud and Abuse in Medicare Part D
- Opioid Use Among Seniors - Issues and Emerging Trends
Last updated March 4, 2021
