2016 National Health Care Fraud Takedown

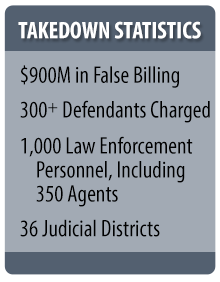
The Department of Health and Human Services Office of Inspector General, along with our state and federal law enforcement partners, participated in the largest health care fraud takedown in history in June 2016. Approximately 300 defendants in 36 judicial districts were charged with participating in fraud schemes involving about $900 million in false billings to Medicare and Medicaid.
Takedowns protect Medicare and Medicaid and deter fraud -- sending a strong signal that theft from these taxpayer-funded programs will not be tolerated. The money taxpayers spend fighting fraud is an excellent investment: For every $1.00 spent on health care-related fraud and abuse investigations in the last three years, more than $6.10 has been recovered.
Graphics Gallery
factsheet-table.jpg bar-graph-figure4-hh.jpg abused-opioids-web.jpg hotspot-map-summary-page.jpgPhoto Gallery
photo01.jpg photo02.jpg photo03.jpgHighlights
- National Health Care Fraud Takedown Results in Charges against 301 Individuals for Approximately $900 Million in False Billing
- Medicare Fraud Strike Force
- Nationwide Analysis of Common Characteristics in OIG Home Health Fraud Cases
- High Part D Spending on Opioids and Substantial Growth in Compounded Drugs Raise Concerns
- Alert: Improper Arrangements and Conduct Involving Home Health Agencies and Physicians
Last updated September 14, 2021
