Report Materials
Why OIG Did This Audit
- Early treatment for autism is important because proper care can reduce children’s difficulties while helping them build on their strengths and learn new skills. Although there are other treatments, applied behavior analysis (ABA) is a commonly used therapy for managing autism symptoms.
- In the past several years, Federal and State agencies have identified questionable billing patterns by some ABA providers and payments to providers for unallowable ABA services.
- Indiana’s fee-for-service (FFS) Medicaid payments for ABA in 2017 were $14.4 million, and by 2020 these payments had increased to $101.8 million—the second highest in the Nation.
- This audit examined whether Indiana’s FFS Medicaid payments for ABA for 2019 and 2020 complied with Federal and State requirements.
What OIG Found
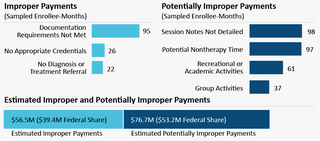
Indiana’s payments for ABA did not fully comply with Federal and State requirements. All 100 sampled enrollee-months included payments for 1 or more claim lines that were improper or potentially improper.
What OIG Recommends
We made several recommendations to Indiana, including that Indiana refund $39.4 million to the Federal Government, provide additional guidance to ABA facilities for documenting ABA, and periodically perform a statewide postpayment review of Medicaid ABA payments to educate providers on requirements. The full recommendations are in the report.
Indiana did not indicate concurrence or nonconcurrence with our recommendations but detailed steps it has taken and plans to take in response to our recommendations.
View in Recommendation Tracker
Notice
This report may be subject to section 5274 of the National Defense Authorization Act Fiscal Year 2023, 117 Pub. L. 263.