Telehealth
Last Updated: 08-07-2023
Generally, telehealth is the remote or virtual delivery of health care services. Patients can receive a wide range of telehealth services, including check-ins with their primary care providers, mental health care, and specialty services. Similarly, telehealth can be provided through a wide range of technologies, including video chats, remote patient monitoring devices, and phone calls. Read more about the types of telehealth.
The Department of Health and Human Services (HHS) has significant influence on how telehealth services are delivered and paid. For example, the Centers for Medicare & Medicaid Services (CMS) establishes payment and coverage requirements for telehealth services in the Medicare and Medicaid programs, and the Office for Civil Rights establishes privacy and security requirements that affect how telehealth services can be delivered.
More on Medicare coverage for telehealth services
More on Medicaid coverage for telehealth services
The COVID-19 pandemic created unprecedented challenges for how patients accessed health care. In response, Congress, HHS, and CMS implemented several flexibilities to expand access to a wide range of services that could be delivered via telehealth. This expansion increased options for health care providers to offer care to beneficiaries enrolled in Federal health care programs, such as Medicare, Medicaid, and the Children's Health Insurance Program (CHIP), remotely during the COVID-19 pandemic.
While the expansion of telehealth has been critical to maintaining beneficiaries' access to care, it is important that new policies and technologies with potential to improve care and enhance access achieve these goals and are not compromised by fraud, abuse, or misuse.
In recent years, the Office of Inspector General (OIG) has conducted dozens of investigations of fraud schemes involving companies and individuals that purported to provide telehealth, telemedicine, or telemarketing services and exploited the growing acceptance and use of telehealth.
OIG encourages Federal health care program beneficiaries and medical providers to be aware of these prevalent schemes. For more information on these fraud schemes, including suspect characteristics related to provider arrangements, please see the Special Fraud Alert: OIG Alerts Practitioners To Exercise Caution When Entering Into Arrangements With Purported Telemedicine Companies.
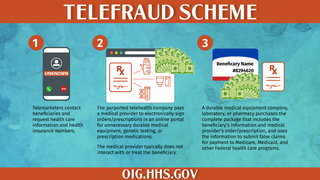
While the facts and circumstances of each case differ, there are some common characteristics of these fraud schemes. For example, telemarketers contact Federal health care program beneficiaries to solicit identifying information related to an individual's health conditions and health insurance number. A purported telehealth company typically then pays a medical provider to review records and electronically sign orders or prescriptions for medically unnecessary durable medical equipment, genetic testing, or prescription medications. The medical provider typically does not interact with or otherwise treat the Federal health care program beneficiary prior to ordering the medically unnecessary items and services. A durable medical equipment company, laboratory, or pharmacy subsequently purchases the complete paperwork package that includes the Federal health care program beneficiary's information and medical provider's order or prescription, and submits false claims for payment to Medicare, Medicaid, and other Federal health care programs.
The following information provides helpful tips that Federal health care program beneficiaries and medical providers can use to distinguish between legitimate telehealth and fraudulent telehealth and telemarketing schemes.
The tips listed below should help you identify fraudulent communications from telemarketers or medical providers. Recognizing these communications as fraudulent could help prevent theft of your personal information and fraudulent billing to Federal health care programs that steals taxpayer money (e.g., billing for medically unnecessary durable medical equipment, genetic testing, or prescription medications).
- Do not provide your Federal health insurance information or other personal information to anyone over the phone, in an email, in a text message, or through social media.
- If someone other than your known medical providers ask for your Federal health insurance information or other personal information, do not provide it. Medical providers that you have received treatment from in the past or that you plan to receive care from in the near future likely already have your insurance information, and typically only ask for it at the time of your previously scheduled appointments.
- If you receive an unsolicited call from a telemarketer or medical provider to discuss information related to your health and you do not recognize the company's name, medical provider's name, or medical group, hang up the phone. Contact your primary care provider and ask for assistance to assess whether the call was legitimate.
- Although each call may be different, typically fraudulent telemarketers will ask about your pain symptoms, your family's history of cancer, or your medications. Do not provide them any information. If you believe you need health care services, contact your primary care provider.
- Another way to handle unsolicited phone calls related to your health is to ask for the caller's name, phone number, and company's name and state that you will call them back. If it is a scammer contacting you, they likely will hang up when you ask for their information.
- Be suspicious of anyone who offers you "free" or "no cost" Medicare or other health care items or services, such as orthotic braces for pain, genetic testing, or prescription creams. Although the Federal health care programs are insurers that pay for items and services, they do not offer or advertise free items and services.
- Medicare and the other Federal health care programs will never call you to offer free or no cost items and services.
- If you receive durable medical equipment (for example, back, knee, or arm braces), genetic or diagnostic testing kits, or prescription medications in the mail, do not accept the delivery unless you verify the order with your established medical provider. Refuse the delivery or return it to the sender. Keep a record of the sender's name and the date you returned the items and report that information to the OIG's fraud hotline.
- Become familiar with the Explanations of Benefits (EOB) and Medicare Summary Notices (MSN) you receive from Medicare and other Federal health care programs. When you notice discrepancies on your EOBs or MSNs, such as names of providers who never treated you or types of medical services that you never received, report it to the OIG's fraud hotline. Additional information from the Senior Medicare Patrol on how to read your EOBs or MSNs.
- Keep available a list of your medical providers' names, locations, and phone numbers so that you may easily recall who your legitimate medical providers are.
- To receive legitimate telehealth services from your provider, seek out family, friends, or caregivers you know and trust to assist with setting up the equipment and other technology needed.
- Educate yourself and talk to your Federal health care program patients about the scope of telehealth services available to them through your office and other legitimate providers.
- Before providing telehealth to patients, verify that the furnishing of the telehealth service via a telecommunications system instead of through an in-person service is clinically appropriate for the service and the patient.
- This verification may include checking with the patient that they have the necessary equipment to participate in telehealth visits.
- Ensure that you are assessing the medical necessity and reasonableness of every item or service that you order or prescribe for a Federal health care program beneficiary.
- Make your patients aware of the types of communications they should expect to receive from your practice.
- Inform your Federal health care program patients that if they receive phone calls or other communications offering them durable medical equipment, genetic testing, diagnostic testing, diabetic supplies, prescription medications, or other health care items or services, they should consult you or another medical provider with whom they already have a provider-patient relationship to determine what, if any, items and services are needed to diagnose or treat their medical conditions.
- You can expect that many of your Medicare patients are receiving unsolicited phone calls offering them "free" medical items and services.
- Be aware of phishing communications, including phone calls or faxes, stating that a clinical team determined that your patients should receive certain items or services and requesting that you approve orders for various items and services.
- Report telehealth fraud to OIG's fraud hotline if you encounter it or if your Federal health care program patients inform you about it.
- For information about how to avoid problematic arrangements when working with entities that provide or purport to provide telehealth, read the Special Fraud Alert: OIG Alerts Practitioners To Exercise Caution When Entering Into Arrangements With Purported Telemedicine Companies.
OIG Law Enforcement Actions Related to Telehealth Schemes
OIG Oversight Work on Telehealth
OIG is conducting significant oversight work assessing telehealth services, including the impact of the public health emergency flexibilities. These reviews provide objective findings and recommendations that can further inform policymakers and other stakeholders considering changes to telehealth policies. This work can help ensure the potential benefits of telehealth are realized for patients, providers, and HHS programs.
Disclaimer
OIG prepared this educational information as a service to the public and it is not intended to grant rights or impose obligations. These educational materials are general summaries and are not legal documents. These materials are not intended to take the place of the written law or regulations. We encourage readers to review the applicable statutes, regulations, and other interpretive materials for a full and accurate statement of their contents. Although every reasonable effort has been made to assure the accuracy of the information within these materials, the ultimate responsibility for complying with the applicable law lies with the provider of services.
This educational information is available on the OIG Web site and you may reproduce, reprint, and distribute it for educational purposes.