Hospice
Last Updated: 01-29-2026
Hospice care is for terminally ill patients who decide to forgo curative treatment and instead receive palliative care. To be eligible, a patient must be certified as having a terminal illness with a life expectancy of six months or less if the illness runs its normal course. Hospice care generally includes nursing and aide services, drugs, and supplies. It may be provided in a variety of settings, such as the patient's home, a nursing facility, or an assisted living facility. About 1.8 million Medicare beneficiaries receive hospice care each year, and Medicare pays about $27.5 billion annually for this care.
What problems has OIG identified with the hospice program?
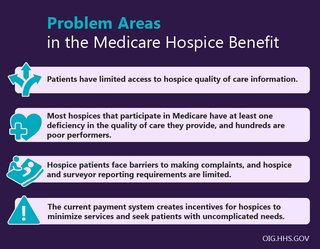
Years of OIG audits, evaluations, and investigations into hospice care have revealed that, while these services can provide great comfort to terminally ill patients and their families, there are significant problems with the program. Our reports and investigations have revealed several concerning issues, including poor—sometimes harmful—quality of care, fraud schemes that involve enrolling beneficiaries without their consent, inappropriate billing practices, limited transparency for patients and their families, a payment system that creates incentives to minimize services, and a rapid growth in the number of new hospices, often to take advantage of these conditions.
To protect hospice patients, OIG conducts extensive audits and evaluations of the hospice program, monitors the impact of program changes, and investigates concerning allegations of fraud and abuse. The key priorities of OIG’s hospice oversight are below.
Ensuring Quality of Care and Preventing Patient Harm
Hospice care should provide patients and their families with comfort and alleviate pain and suffering. However, OIG evaluations and investigations have revealed some concerning patterns of poor quality of care and instances of serious harm to patients. Most hospices that participate in Medicare have at least one "deficiency" in the quality of care they provide, and hundreds are considered poor performers. Some of these deficiencies include leaving patients in unnecessary pain and discomfort for days, failing to screen employees for prior abuse and neglect, and failing to properly train staff.
OIG has recommended changes to promote quality of care and prevent patient harm. These changes include increasing oversight of hospices with a history of serious deficiencies, strengthening requirements to report abuse and neglect, and creating user-friendly mechanisms for patients and families to submit complaints.
OIG also investigates allegations of fraud and abuse, to ensure that fraudulent providers are held accountable for taking advantage of this valuable program. Our investigations have identified harmful and concerning providers resulting in numerous criminal, civil, and administrative enforcement actions.
Building Transparency and Access to Information
Patients and their families and caregivers deserve accurate and reliable information about hospice performance so they can compare providers and make the best decisions for their care needs. Unfortunately, CMS's Hospice Compare website has significant gaps of information and does not provide a full picture of the quality and performance of different hospice providers.
Developing and disseminating additional information on hospices to help patients and their families make informed choices is a key priority for OIG. We have recommended that CMS include information about complaints filed and resulting deficiencies, as well as survey reports from State agencies and accrediting organizations, on Hospice Compare. We also have recommended adding information about the average number and types of services a hospice provides, how often physicians visit, and how often a hospice provides services on weekends.
Promoting Accurate and Effective Billing Practices
One important way to maintain the integrity of health programs and services is to ensure that providers are driven by their patient's needs and best interests. Hospice programs, however, have a payment structure that often undermines this basic principle. A hospice is paid every day a patient is in its care, regardless of the quantity or quality of services provided. This creates financial incentives for providers to minimize services and seek patients who have uncomplicated needs.
OIG has recommended that CMS take steps to tie payment to patient needs and quality of care, seeking statutory authority if necessary. These changes, coupled with strengthened oversight measures, would help ensure that services rendered adequately serve patients.
What more needs to be done to improve hospice care?
The Consolidated Appropriations Act of 2021 included a number changes to improve hospice care. While the Act addressed several of OIG’s long-standing hospice recommendations, more needs to be done. Many of the changes required by the Act are not yet in practice, and there are still many OIG recommendations that have not been implemented. These include changing the payment structure, increasing oversight by improving the survey process, and using available data to target oversight most effectively. OIG has also recommended that CMS study whether additional items and services could be included within the hospice benefit, to ensure that hospice care is comprehensive.
Click below to view our open recommendations on hospice by report.
View report | 4 open recommendations
- CMS should expand the deficiency data that accrediting organizations report to CMS and use these data to strengthen its oversight of hospices.
- CMS should include on Hospice Compare the survey reports from accrediting organizations, once authority is obtained.
- CMS should increase oversight of hospices with a history of serious deficiencies.
- CMS should include on Hospice Compare the survey reports from State agencies.
View report | 1 open recommendation
- CMS should monitor surveyors' use of immediate jeopardy citation.
View report | 10 open recommendations
- CMS should take appropriate actions to follow up with hospices that engage in practices or have characteristics that raise concerns.
- CMS should develop and execute a strategy to work directly with hospices to ensure that they are providing drugs covered under the hospice benefit as necessary and that the cost of drugs covered under the benefit are not inappropriately shifted to Part D.
- CMS should include on Hospice Compare deficiency data from surveys, including information about complaints filed and resulting deficiencies.
- CMS should ensure that a physician is involved in the decisions to start and continue general inpatient care.
- CMS should increase oversight of general inpatient care claims and focus particularly on general inpatient care provided in SNFs, given the higher rate at which these stays were inappropriate.
- CMS should assess the current payment system to determine what changes may be needed to tie payments to beneficiaries’ care needs and quality of care to ensure that services rendered adequately serve beneficiaries’ needs.
- CMS should adjust payments based on these analyses, if appropriate, to ensure that the payment system is aligned with beneficiary needs and quality of care.
- CMS should work with its partners, such as hospitals and caregiver groups, to make available consumer-friendly information explaining the hospice benefit to beneficiaries and their families and caregivers.
- CMS should modify the payments for hospice care in nursing facilities.
- CMS should analyze claims data to identify hospices that engage in practices or have characteristics that raise concerns.
View report | 1 open recommendation
- CMS should provide guidance to hospices regarding the effects on beneficiaries when they revoke their election and when they are discharged from hospice care.
Resources for Patients and Families
- Know Your Rights, Take Action
- Eye on Oversight: Hospice
- Fact Sheet: Protecting Hospice Beneficiaries
- Report Suspected Fraud, Waste, and Abuse
Featured Reports
- Safeguards Must Be Strengthened To Protect Medicare Hospice Beneficiaries From Harm
- Hospice Deficiencies Pose Risks to Medicare Beneficiaries
- Vulnerabilities in the Medicare Hospice Program Affect Quality Care and Program Integrity: An OIG Portfolio
- Medicare Payments of $6.6 Billion to Nonhospice Providers Over 10 Years for Items and Services Provided to Hospice Beneficiaries Suggest the Need for Increased Oversight
- Medicare Part D Is Still Paying Millions for Drugs Already Paid for Under the Part A Hospice Benefit
- Medicare Improperly Paid Suppliers an Estimated $117 Million Over 4 Years for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies Provided to Hospice Beneficiaries